In the bacterial form, bacteria enter the meningeal space and elicit an inflammatory response. This process includes the release of a purulent exudate that is spread to other areas of the brain by the cerebrospinal fluid (CSF). If it is left untreated, the CFS becomes thick and blocks the normal circulation of the CFS, which may lead to increased intracranial pressure (ICP) and hydrocephalus. Long-term effects of the illness are predominantly caused by a decreased cerebral blood flow because of increased ICP or toxins related to the infectious exudate. If the infection invades the brain tissue itself, the disease is then classified as encephalitis. Other complications include visual impairment, cranial nerve palsies, deafness, chronic headaches, paralysis, and even coma.
Meningitis is most frequently caused by bacterial or viral agents. In newborns, Streptococcus pneumoniae is the most frequent bacterial organism; in other age groups, it is S. pneumoniae and Neisseria meningitidis. Haemophilus influenzae is the most common organism in unvaccinated children and adults who contract meningitis. Viral meningitis is caused by many viruses. Depending on the cause, isolation precautions may be indicated early in treatment. There has been a decrease in viral meningitis in locations where immunizations have become routine.
Nursing care plan assessment and physical examination
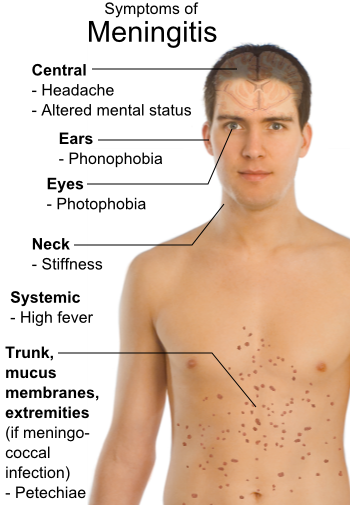
The history varies according to which form of meningitis the patient has: acute or subacute. For the subacute form, the patient or family may describe vague, mild symptoms such as irritability, loss of appetite, and headaches. With an acute infection, there may be reports of a headache that became progressively worse, with accompanying vomiting, disorientation, or delirium. The patient may also note an increased sensitivity to light (photophobia), chills, fever, and even seizure activity. Frequently the patient or family describe a recent upper respiratory or other type of infection. A patient with pneumococcal meningitis may have had a recent ear, sinus, or lung infection or endocarditis. It is sometimes associated with other conditions, such as sickle cell disease, basilar skull fracture, splenectomy, or alcoholism. H. influenzae meningitis is also associated with lung and ear infections.
Classically, the signs of meningitis are progressive headache, high fever, vomiting, nuchal rigidity (stiff neck that creates pain when flexed toward chest), and change in the patient’s level of consciousness or disorientation. Other signs include photophobia (sensitivity of eyes to light), a positive Kernig’s sign (inability to extend legs fully when lying supine) and Brudzinski’s sign (flexion of the hips when neck is flexed from a supine position), and seizures. Some patients develop signs of increased ICP, such as mental status deterioration with restlessness, confusion, delirium, stupor, and even coma. Patients often experience visual changes; during ophthalmoscopic examination, you may note papilledema and unreactive pupils. Examine babies for bulging fontanels; nuchal rigidity may not be present if the An ongoing assessment throughout the patient’s hospitalization is important to detect changes in the condition. Serial monitoring for symptoms such as head and neck pain, vomiting, fever, and alterations in fluid and electrolytes is essential. Neurological assessments are completed at timely intervals (every 1 to 2 hours or as indicated by the symptoms), and changes are reported to the physician when appropriate.
Provide ongoing evaluations to determine the anxiety level and need for information and support. Anxiety is generally present any time there is an illness associated with the brain. Note that some patients or parents feel guilty because of some delay in accessing the healthcare system. Family members may be particularly upset if they witness a seizure.
Nursing care plan primary nursing diagnosis: Infection related to pathogens in the Cerebrospinal fluid.
Nursing care plan intervention and treatment plan
The most critical treatment is the rapid initiation of antibiotic therapy. In addition, assessment and maintenance of airway, breathing, and circulation (ABCs) are essential. Treatment with intubation, mechanical ventilation, and hyperventilation may occur if the patient’s airway and breathing are threatened. Serial neurological assessments and vital signs not only monitor critical changes in the patient but also monitor the patient’s response to therapy. Supportive measures such as bedrest and temperature control with antipyretics or hypothermia limit oxygen consumption. Gradual treatment of hyperthermia is required to prevent shivering.
Other strategies to manage increased ICP include osmotic diuretics, such as mannitol, or intraventricular CSF drainage and ICP pressure monitoring. Fluids are often restricted if signs of cerebral edema or excessive secretion of antidiuretic hormone are present. If the patient experiences seizures, the physician prescribes anticonvulsant medications. Surgical interventions or CSF drainage may be required to prevent permanent neurological deficits as a result of complications such as hydrocephalus or abscesses. The patient is likely to have a severe headache from increased ICP. Because large doses of narcotic analgesia mask important neurological changes, most physicians prescribe a mild analgesic to decrease discomfort. In children, pain relief decreases crying and fretting, which if left untreated, have the potential to aggravate increased ICP.
Rehabilitation begins with the acute phase of the illness but becomes increasingly important as the infection subsides. If residual neurological dysfunction is present as a result of irritation, pressure, or brain and nerve damage, an individualized rehabilitation program with a multidisciplinary team is required. Vision and auditory testing should be done at discharge and at intervals during long-term recovery because early interventions for these deficits are needed to prevent developmental delays.
Make sure that the patient has adequate airway, breathing, and circulation. In the acute phase, the primary goals are to preserve neurological function and to provide comfort. The head of the bed should be elevated 30 degrees to relieve ICP. Keep the patient’s neck in good alignment with the rest of the body and avoid hip flexion. Control environmental stimuli such as light and noise, and institute seizure precautions. Soothing conversation and touch and encouraging the family’s participation are important; they are particularly calming with children who need the familiar touch and voices of parents. Children are also reassured by the presence of a security object.
Institute safety precautions to prevent injury, which may result from either the seizure activity or the confusion that is associated with increasing ICP. Take into account an increase in ICP if restraints are used and the patient fights them. Implement measures to limit the effects of immobility, such as skin care, range-of-motion exercises, and a turning and positioning schedule. Note the effect of position changes on ICP, and space activities as necessary.
Explain the disease process and treatments. Alterations can occur in thought processes when ICP begins to increase and the level of consciousness begins to decrease. Reorient the patient to time, place, and person as needed. Keep familiar objects or pictures around. Allow visitation of significant others. Establish alternate means of communication if the patient is unable to maintain verbal contact (e.g., the patient who needs intubation). As the patient moves into the rehabilitative phase, developmentally appropriate stimuli are needed to support normal growth and development. Determine the child’s progress on developmental tasks. Make appropriate referrals if the child is not progressing or if the child or family evidence signs of inability to cope.
Nursing care plan discharge and home health care guidelines
Explain all medications and include the mechanism of action, dosage, route, and side effects. Explain any drug interactions or food interactions. Instruct the patient to notify the primary healthcare provider for signs and symptoms of complications, such as fever, seizures, developmental delays, or behavior changes. Provide referrals and teaching specific to the identified neurological deficits. Encourage the parents to maintain appropriate activities to facilitate the growth and development of the child.
No comments:
Post a Comment