Sunday, December 31, 2006
Saturday, December 30, 2006
Travel Nurse: Assignment in Tallahassee

We enjoyed our visit so much we've decided to take a travel nurse assignment in Tallahassee, Florida for the next few months. My husband is a big Florida State fan but I doubt we will be here long enough for the next football season to start.
I will be working at one of the two main hospitals in Tallahassee. The winter weather here is relatively mild compared to some of my other travel nurse assignments. The temperature has been in the 60's for the last few weeks (including Christmas Day) which is something I can certainly get used to.
We found a home in a suburb of Tallahassee to stay in while I complete my assignment. I am still working out the housing stipend details with my travel nurse agency.
I start work next week. Wish me luck.
Tuesday, December 26, 2006
A Nurse's Christmas Poem
The Lasix was filling the Foleys galore.
Stockings were worn to prevent emboli.
They came in two styles: knee- and thigh-high.
The patients were nestled half-assed in their beds,
While visions of stool softeners danced in their heads.
We in our scrubs, and they in their gowns -
Fashions created to hide extra pounds.
When down in the E.R. it became such a zoo.
They called for admissions for me and for you.
They're coming, they're going, they're looking the same.
My patience for patients is starting to wane.
Now call lights are ringing, the patient expounds
"I have not had my peri-care, please send someone down."
So now delegation seems like a good plan.
We pass on to others the needs of this man.
When, what to my wondering eyes should appear
But Santa himself and 8 tiny reindeer.
He states that he came in from Central Supply
To bring us LR, NS, and D5.
The doctors then scribbled what no one could read.
Orders for patients, to measure their pee.
We try to decipher illegible words.
Orders for patients, to guiac their turds.
The new shift arriving, our day is now through.
How'd the stool and the emesis get in my shoe?
We give them report and pass on the facts,
And tell them of Duoderm lining the cracks.
And the Nurses exclaimed as they drove out of sight,
"Ambien to all! And to all a good night!"
Monday, December 25, 2006
MERRY CHRISTMAS!
Sunday, December 24, 2006
Friday, December 15, 2006
ok, time for some serious sleeping in!

The semester is over, got through the OSCEs in one peice (barely!) and I am now ready to sleep in, relax and strart revising notes for next semester (yes yes I know, I am on vacation). I have made it through yet another semester and still cannot believe that I have made it half-way through nursing school.
WOW!
Mental Health Carols
2. Multiple Personality Disorder -- We Three Kings Disoriented Are
3. Dementia -- I Think I'll be Home for Christmas
4. Narcissistic -- Hark the Herald Angels Sing About Me
5. Manic -- Deck the Halls and Walls and House and Lawn and Streets and Stores and Office and Town and Cars and Buses and Trucks and Trees and.....
6. Paranoid -- Santa Claus is Coming to Town to Get Me
7. Borderline Personality Disorder -- Thoughts of Roasting on an Open Fire
8. Personality Disorder -- You Better Watch Out, I'm Gonna Cry, I'm Gonna Pout, Maybe I'll Tell You Why
9. Attention Deficit Disorder -- Silent night, Holy oooh look at the Froggy - can I have a chocolate, why is France so far away?
10. Obsessive Compulsive Disorder -- Jingle Bells, Jingle Bells, Jingle Bells, Jingle Bells, Jingle Bells, Jingle Bells, Jingle
Bells, Jingle Bells, Jingle Bells, Jingle Bells, Jingle Bells, Jingle Bells, Jingle Bells, Jingle,Bells, Jingle Bells, Jingle Bells, Jingle
Bells, Jingle Bells, Jingle Bells, Jingle Bells, Jingle Bells, Jingle Bells, Jingle Bells, Jingle Bells, Jingle Bells, Jingle Bells, Jingle
Bells, Jingle Bells, Jingle Bells, Jingle Bells, Jingle Bells, Jingle Bells, Jingle Bells, Jingle Bells, Jingle Bells, Jingle Bells, Jingle
Bells...
Thursday, December 14, 2006
All Dressed Up!
OSCE
Last day is tomorrow, we have OSCEs, 6 of them then I have a month off. YAY! In the meantime the stress is high and we are all stressed out. To make matters worse, my hip hurts, my BP is in the toilet (too low), my pulse is tachycardic (great) and my neuro wants me to do a sleep study (among other thinsg) and all I want to do right now is crawl under a rock and HIDE. I am just so fed up with school and need a break so badly. I am afraid of failing the semester (about 1/2 of us are in the same boat, so at least I am not alone). I have to do well on the OSCE if I don't want crap grades this semester.
You may wonder, What is an OSCE? It stands for "Objective Structured Clinical Examination". Basically they give you a scenario and you have to act it out, describing what you are doing and why. Talk it out and do the necessary skills. That's how you get the points. Scary shit at times. So far I have always managed a good grade, but this term we have 6 of them for our final and we're not entirely sure what they will ask us! We have to do it in uniform too... odd.
So any of you out there reading this, cross your fingers for me and wish me luck!
Friday, December 8, 2006
Travel Nurse: Assignment in St. Augustine, FL

Last year I worked as a travel nurse in St. Augustine, Florida. St. Augustine is generally recognized as the oldest city in the United States and is full of history. Downtown St. Augustine has old cobble stone streets lined with beautiful European style cathedrals. I took a picture of this cathedral during one of our family Sunday afternoon strolls. There are at least a dozen more similar cathedrals.

There is also a street near the cathedrals called "St. George Street" with a bunch of olde world Spanish styled specialty shops. At the end of St. George Street is an old schoolhouse with a sign reading "The Oldest Wood School House In The U.S.A. St. Augustine Florida." I told my two sons that if they didn't start doing better in school we are going to start sending them to that school house.
My travel nurse assignment in St. Augustine was easily one of the most interesting I have taken. As far as the work itself, most of my patients were elderly, retired people who were either extremely pleasant or extremely cantankerous. The work facilities were modern and the computer systems were state of the art. There is not a lot of traffic in St. Augustine which makes traveling to and from the hospital easy.
I would recommend St. Augustine to any travel nurse who likes visiting historical sites. I would be remiss if I did not at least mention the Spanish Fort across the street from St. George street. Students from the nearby Flagler College walk to the fort and lay out in the sun on the open green spaces surrounding the fort. My sons also want me to mention that the fort has a cool moat that they believe once held sharks and alligators at the same time.
Thursday, December 7, 2006
Regents approve nursing admission cuts
Wednesday, December 6, 2006
Julie's picks from the Nursing Literature Nov 2006
 SJH/CHOC employees can access these article through Burlew Medical Library.
SJH/CHOC employees can access these article through Burlew Medical Library.Bedard D. Purden MA. Sauve-Larose N. Certosini C. Schein C. The pain experience of post surgical patients following the implementation of an evidence-based approach. [Journal Article, Research, Tables/Charts] Pain Management Nursing. 2006 Sep; 7(3): 80-92. (34 ref)
McKnight M. The information seeking of on-duty critical care nurses: evidence from participant observation and in-context interviews. [Journal Article, Research, Tables/Charts] Journal of the Medical Library Association. 2006 Apr; 94(2): 145-51.
Drenning C. Using the best evidence to change practice. Collaboration among nurses, advanced practice nurses, and nurse researchers to achieve evidence-based practice change. [Journal Article] Journal of Nursing Care Quality. 2006 Oct-Dec; 21(4): 298-301. (17 ref) Burlew carries this journal
Jackson R. Ameratunga S. Broad J. Connor J. Lethaby A. Robb G. Wells S. Glasziou P. Heneghan C. EBN notebook. The GATE frame: critical appraisal with pictures. Evidence-Based Nursing. 2006 Jul; 9(3): 68-71. (7 ref)
Oermann MH. Floyd JA. Galvin EA. Roop JC. Brief reports for disseminating systematic reviews to nurses. Clinical Nurse Specialist. 2006 Sep-Oct; 20(5): 233-40. (33 ref)
Gobel BH. Beck SL. O'Leary C. Nursing-sensitive patient outcomes: the development of the Putting Evidence Into Practice resources for nursing practice. Clinical Journal of Oncology Nursing. 2006 Oct; 10(5): 621-4, 641-3. (9 ref
Galligan M. Proposed guidelines for skin-to-skin treatment of neonatal hypothermia. MCN: The American Journal of Maternal/Child Nursing. 2006 Sep-Oct; 31(5): 298-306. (29 ref) Burlew carries this journal
Lake ET. Cheung RB. Are patient falls and pressure ulcers sensitive to nurse staffing? Western Journal of Nursing Research. 2006 Oct; 28(6): 654-77. (39 ref) Burlew carries this journal
Delmas L. Best practice in the assessment and management of diabetic foot ulcers. Rehabilitation Nursing. 2006 Nov-Dec; 31(6): 228-34. (55 ref) Burlew carries this journal
Helberg D. Mertens E. Halfens RJG. Dassen T. Treatment of pressure ulcers: results of a study comparing evidence and practice. Ostomy/Wound Management. 2006 Aug; 52(8): 60-3, 66, 68 passim. (25 ref) Burlew carries this journal
Tuesday, December 5, 2006
Something I had to share
#10 is especially pertinent to me and my classmates at the moment...
It's time...to impart wisdomses!
1. If you tell a resident that you'll take care of bowel management for them, not only will he or she sign anything you write, s/he'll love you forever.
2. Don't call at 0300 for a sleeping pill for a patient.
3. White is a magnet for ook of all sorts.
4. Your favorite clogs have just been discontinued, and your favorite pen is about to run out of ink.
5. The cutest bartender is always taken.
6. There is no substitute for dental floss.
7. The volume of ook that will splatter on you is directly proportionate to how much you like the scrubs you're wearing.
8. The doctor who yells at you is actually trying to make up for the size of his or her genitalia. Don't let it rattle you.
8a. Remember that you can go home at seven; they're on call. Smile.
9. The word "pomegranate" never looks like you've spelled it right.
10. If you're a student, don't fret: you'll never use care plans again.
Sunday, December 3, 2006
Rude, Obnoxious, Incompetent...
We had problems with my mom's PICC line and I called the CLSC to tell them what we needed, we were reassured that the nurse coming to the house would have all she needed... well she came and HAD NO IDEA what to do! She looked tha the PICC line as if it was the first time she had seen one and wondered why they would send my mom home with it! OMG! I had to bite my tongue and not react, I was so mad. At least she had the foresight to bring along another nurse later on who knew what to do. She was younger and was more personable and spoke to me like I had a brain and not like I was an ignorant 12 year old.
Strange huh? (considering her experience).
Hope we don't get her again!
Saturday, December 2, 2006
It's almost over
I enjoyed it, would've liked it more if I had had more than 3 weeks in the hospital... this community placement sucks rocks for the most part, though it was less work I suppose.
I am starting to panic, have 3 assigments due Monday, a Bio test Monday, a teaching & learning presentation due Thursday, and a nursing test Friday. Then Friday AFTER the test I have to get my ass to Salem, Mass. for a wedding (I am a bridesmaid). Then the following Tuesday I have the Bio final Exam (and when am I studying for that???) and then Friday the nusring final OSCEs (oh joy!).
Have I mentioned I am freaking out?
Sunday, November 26, 2006
Misuse of Resources
I often speak passionately to others about my calling. But this weekend, while I was visiting extended family and friends, I was somewhat deflated by their questions about my career. "Why aren't you going to medical school?" they'd ask.
I made a bunch of standard arguments, mostly centered around the saying "Doctors cure but nurses care". I explained that my desire is to work with people holistically and individually. I want to be present. And I am far more interested in the human elements of health care than the scientific ones. While doctors can do those things, nursing just feels like the best fit.
But none of these arguments seemed to phase them. They couldn't grasp why I'd become a nurse instead of a doctor when I was obviously bright enough to be the latter. They cited a myriad of reasons it would be better for me--most of which boiled down to a supposedly "superior lifestyle". But the one thing that really stuck with me was the phrase "Just wait, you will always be subject to people who are less than you."
I can't help but be upset by the entire perspective. It feels wrong on so many levels.
For one, I don't think a "smart person" going into nursing should be seen as a waste! If I succeed--and I plan to--it will only do credit to the profession, not discredit me. For another, I don't think money is a good reason to choose any career. And perhaps I am naive, but I haven't exactly found nurses to be totally subject to doctors. Nurses seek to be collaborators in patient care; this is the meaning of professionalism. True, some physicians still try to walk all over supportive staff. But people who work in hospitals know it's far less challenging to work with doctors than it is to work with patients! "Subject to those less than you"? Obviously! (Just not how you'd think!)
It's very discouraging to be told that you are, in essence, misapplying your potential. But the thing I think others are overlooking is the fact that my gifts aren't limited to the deduction logical puzzles or the intuitive grasp of certain subjects. So what if I took a test when I was a child that indicated I had some above-average abilities? I have developed others as an adult that are far more important to a meaningful life. They're the more immeasurable qualities of the heart... they compel me to extend my hand to strangers and to listen with compassion. I may not always succeed, but I am a person who is not only able, but willing!
Surely that means more than the money I could have made or the power I could have held. It's not a lack of ambition that set me on this path. It's because I feel like if I place more value on relationships than the other factors, I can't really go wrong. I will have enough money and responsibility. But I will have an abundance of friendship and respect.
Again, it is totally possible for doctors to be and do all the things I describe in addition to their regular jobs. But for nurses, that thing is their job. I watch them while I work. I see what each professional does. And I don't regret my choice, not even a little. Because I know who and what I am.
Wednesday, November 22, 2006
Resarch Study and Commentary by Dana Rutledge, Phd, RN, Nursing Research Facilitator
Schulman-Green, D. et al. (2005). Unlicensed staff members’ experiences with patients’ pain on an inpatient oncology unit. Implications for redesigning the care delivery system. Cancer Nursing, 28, 340-347. Staff at SJO/CHOC can access the full text of this article through the library's web site.
Authors’ Abstract
Although unlicensed staff have routine contact with patients in pain, little research relates to their role with these patients. The purpose of this study was to describe the experiences of unlicensed inpatient hospital staff caring for cancer patients in pain. We sought to understand pain identification and communication practices, describe common practice sitaut9on, and identify training needs. We conducted 4 focus groups with unit secretaries, nurses’ aides, and housekeepers (n = 24) on 2 inpatient oncology units at an urban, northeastern teaching hospital. Group processes were tape-recorded, transcribed, and analyzed using Atlas/ti software and content analysis. Analysis generated 5 issues related to pain in the daily practice of unlicensed staff: perceived function with pain, building relationship with patients, interpreting patients’ pain, system issues, and job challenges and coping strategies. Unlicensed staff reported performing important functions related to pain, including alerting nursing staff to patients’ pain, and providing psychosocial support. Participants shared difficulties of working with patients in pain an expressed interest in education on pain identification and course of illness. Findings provide insight into the role of unlicensed staff, and have implications for the educational preparation of this group as well as the nature of their participation in the care delivery system.
Commentary by Dana Rutledge, PhD, RN, Nursing Research Facilitator
In this qualitative study, researchers described results of focus groups of unlicensed hospital staff who were asked about experiences with patient and pain. Nurses might be surprised at some of the important ways these staff perceive that they impact pain and its management. Patient care assistants (14, the largest group of staff) noted that they were assessing pain using the 0 – 10 score at the time they did vital signs. They reported having difficulty identifying the nature of pain when patients found the 0-10 scale confusing or difficult to respond to. Is this a problem that could occur at St. Joseph?
Those interviewed mentioned their roles in assisting in patient comfort by giving emotional and physical care. Some use nonpharmacologic pain management techniques such as distraction or listening. These staff members consider comfort care important to their roles. Most unlicensed staff reported communicating patient pain to nursing staff, and consider this one of their most important roles.
As with nurses, unlicensed staff identified challenges to dealing with patients’ pain. One was their overall heavy workloads, which interfered when they wanted to spend time with patients in pain. They emphasized the importance of teamwork, individualizing care, and empathy in caring for their patients.
In the discussion of their results, Schulman-Green and colleagues suggest that care redesign that enhances PCA-nurse relationships, expands training for unlicensed staff, and debriefing at intervals would improve pain management for patients in pain. What do you think?
Tuesday, November 21, 2006
BP?
NPA
I had a 20 day old baby boy, in for rule out sepsis and possible meningitis. The MD asked for us to do an NPA (naso-pharyngeal aspiration) and my co-assigned RN let me do it! I was with my clinical instructor and 2 classmates and man was I nervous! BUT did not let it show... as both parents were there. It was the first time I was doing this procedure on a live person, let alone a baby!
Managed to do it without incident and we got the sample and sent it to the lab. No idea what the results are though as we had to leave.. hope the little guy is ok.
Can't wait to do more skills like that.

"Nasopharyngeal Aspiration for Respiratory Virus or Bacterial Testing
Requires a suction mechanism (syringe, vacuum pump or wall suction), a specimen trap and catheter.
Insert catheter nasally into posterior nasopharynx.
Apply suction as catheter is slowly withdrawn. Do not leave sample in tubing.
If sample has been aspirated into a syringe seal the end of the aspiration tube and send specimen in syringe
or wash aspirate through tubing or trap with:
• 3mL of virus transport medium if for viral diagnosis only
• 3mL of sterile saline for microbiology culture/sensitivities and or viruses
Place sample in transport medium into sterile transport vial.
Ensure that the top of the vial is screwed on securely.
Label with patient name, date of birth, sample type and date of collection."
Friday, November 17, 2006
who me? ...Uncoordinated?
Damn I can't walk and drink coffee at the same time.. wonder if I can still walk and chew gum at the same time!
Wednesday, November 8, 2006
St. Joseph Hospital PACU Nurses Win Poster Presentation Award

Tracy Dickman, RN, BSN, Clinical Nurse II, Pavilion PACU, Darlene Soriano, BS, MHA, Surgery Support Specialist, Pavilion, OR, and Dana Rutledge, RN, PhD, Nursing Research Facilitator, won first prize among 14 other presentations for a nursing research poster at the recent Joint Southern California STTI Chapters Odyssey 2006 Conference.
This prestigious honor was bestowed along with a plaque at the Ontario conference October 26-27. The poster presentation described an action research project carried out in the Pavilion PACU.
During Fall 2005, Alicia Leal, BSN, RN, CPAN and other PACU staff initially designed the research study that examined patient flow within the Surgery Center. Tracy analyzed the statistical data collected and noticed a potential clinical problem. Tracy then met with Kathy Dureault, RN, MSN, Clinical Educator. Many patients were arriving unprepared to ambulatory surgery (e.g., did not have transportation home or a responsible adult to be with them upon discharge, etc.). Kathy connected Tracy with Dr. Rutledge, who discussed how to evaluate the nature and intensity of the problem using survey methodology.
PACU nurses implemented an action research project. They found that in over 600 patients admitted for surgery, 75% had received the Personal Recovery Plan Pamphlet (PRPP) developed by SJO nurses and disseminated through surgeon’s offices. In all patients who received it, the Plan was perceived as helpful. Of the patients, 78% received a preoperative call from SJO staff. Despite not all patients receiving the pamphlet or call, 99% of patients thought that their preparation for surgery was adequate.
During fall 2006, Darlene called surgeon’s offices, making sure staff understood how the PRP was to be used. She updated and converted them into electronic files available of the English, Vietnamese, and Spanish versions to enable staff to keep copies readily available in offices. The PRP is also now available on the SJO Intranet/website at http://www.sjo.org/ under the Patients and Families link. You can also view the Personal Recovery Plan Pamphlet here. Between Thanksgiving and Christmas, Tracy and PACU nurses will be surveying patients again to determine proportions of patients who have been adequately prepared for their surgeries. They hope to see a change.
Implementing a Sedation Protocol for Ventilated Patients
Victoria discussed the practice change in progress in the Intensive Care Unit. You can review her complete PowerPoint here.
Group Visits for Diabetes Management
Teresa educated the audience on “Shared Medical Appointments” and specifically a group at La Amistad focused on diabetes management that started November 2005. An added bonus to her group was the inclusion of family members who could also reinforce the education presented at these group visits. You can view her PowerPoint here.
Five-Minute e-mail Nursing Journal Club
Monday, November 6, 2006
SJH Action Research: Decreasing Incidence of Bleeding and Hematoma Formation in New Fistulas
Investigators:
Carmeleene Baguio MSN, RN Vascular Access Coordinator Renal Center, Dr. Amer Jabara, Renal Center Medical Director, Dialysis Staff in the Outpatient chronic hemodialysis unit
Problem identified:
Bleeding and subsequent hematoma on new fistulas when initially used for hemodialysis. When this occurs the fistula is allowed to rest for 2 weeks. This allows the hematoma and bruising to resolve. Sometimes it takes longer than 2 weeks or the hematoma needs surgical evacuation. This delays the use of the fistula and increases the risk of the fistula failure.
Purpose of the project:
To investigate the factors or reasons that cause excessive bleeding when new fistulas are initially used.
Evidence/Research:
The arteriovenous fistula (AVF) is the “gold standard) for vascular access. Fistulas have the longest longevity (75% working at 3 years, least likely to be infected (35x less than central venous catheters, 10x less than grafts), and lowest mortality (3x less than central venous catheters).
The Kidney Disease Outcomes Quality Initiative (National Kidney foundation, 2001) and the American Nurses Nephrology Association (ANNA) Standards and Guidelines of Clinical Practice for Nephrology Nursing recommend the AVF as the first choice of access.
The Fistula First Initiative recommends that 66% of patients on chronic hemodialysis use fistula as their primary access by year 2009.
Evidence shows that skill is required in creating and cannulating new fistulas.
28-53% of fistulas never mature to support dialysis ( Beathard, 2006 American Society of Nephrology)
According to Brouwer, 2003 a new fistula must be treated with great care to prevent damage. The goal is to help the access to mature into a long-term lifeline for the patient. She has recommended some guidelines in the care of this new fistula.
Several factors impact effectiveness of fistula placement and function. A multidisciplinary approach to evaluating and managing fistula maturation increases the chance of success.
Action Plan:
I discussed this problem with St. Joseph Hospital research council chair, Dana Rutledge, Dr. Jabara, Medical director of the Renal Center, the experienced dialysis nurses and technicians to get input on how what they thought was causing this problem. Based on current guidelines in the successful use of new fistulas a data collection tool was created to collect retrospective and prospective data on patients with new fistulas. This information consisted of possible factors that could affect bleeding and subsequent hematoma when new fistulas are initially used.
Retrospective and prospective data was collected on patients that had new fistulas that were being used for the first time. I informed the staff of what the plan was to address this problem.
During the data prospective data collection the staff was aware to check patient’s heparin dose based on the ACT’s, coumadin and other oral blood thinners that patient might be taking, patient education on holding needle sites post dialysis. As Vascular Access coordinator, I collected the data and facilitated patient referral to Interventional Radiology or vascular surgeon. I also did staff and patient education in the clinical area while data was being collected.
Outcomes:
Data was collected on six retrospective and six prospective patients that had new fistulas. Data included: Age of fistula when initially used, needle size used, heparinization during dialysis, other anticoagulants that patient was on, activated clotting times (ACTs), other bleeding issues, patient medical history associated with hematologic disorders, prescribed and/or complementary or alternative medications used by the patient and physical examination of the fistula.
Chart review was done using the data collection tool. Retrospective data showed that four of these patient’s ACTs were prolonged. Two were on coumadin, and two patients had narrowing of the fistula. Heparin dose was adjusted according to the ACT result.
For the prospective patients, heparin dose was evaluated and adjusted based on the ACT’s. This was done prior to using the fistula for the first time. Four of the patients did not have any bruising after the fistula was initially used. Two had minor bruising. This was related to needle manipulation since the fistula was not mature to support dialysis.
How is this significant?
There was a significant decrease in the incidence of bleeding after new fistulas were used for the first time.
Recommendations:
There will be an increase of new fistulas as a result of the Fistula First Initiative.
Systematic assessment of the new fistula before first use is imperative. Using the data collection tool created for this research will be useful in assessment of new fistula.
Patient and staff education on care of fistula and graft infiltrations to promote longevity in the use of these accesses.
Knowledge and Attitudes of SJH Nurses on Pain and Management
Travel Nurse: Checklist (Housing Stipend)
HOUSING
Ask the agency:
1) What kind of housing is being offered, private or shared?
2) If shared, can I request a nonsmoking roommate or a roommate that works the same shift as I do?
3) Where is the housing located and when can I move in?
4) Can I get a housing stipend if I live in a home I have purchased in my new assignment area, live out of town with friends or relatives, or rent a home on my own while on assignment?
5) If the travel agency offers a stipend to pay for utilities, when is it paid and is it taxed?
6) Does the assignment I'm considering offer free private housing?
7) Can I take my spouse, significant other, children or pets without any additional charges?
8) Is the house or apartment furnished?
Finally, from all the research I've done, the most important bit of advice I can give is that everything should be included in a written contract. What sounds too good to be true probably is, and the only way for us to be sure we will get all the things we've been told we will get, is to have it put in writing. We should ask our recruiter and the facility to put down on paper the things that are most important to us (if they haven't already). There are lots of agencies and millions of facilities out there, we should be a ble to get what we are looking for and we shouldn't have to settle for less.
Wednesday, November 1, 2006
Travel Nurse: Checklist (Work Facility)
YOUR FUTURE WORK FACILITY
Ask the agency:
1) Has the facility used travel nurses before?
2) What is the nurse/patient ratio per shift?
3) Will there be unlicensed staff or other ancillary staff in the unit?
4) What type of scheduling is done (weekly, monthly, quarterly)?
5) Will I work in 4, 8, or 12 your shifts?
6) What are the facility's orientation procedures?
7) Are study guides provided and testing required?
8) Are there any licensure issues?
9) What type of charting system is used?
10)Do travelers float first and, if so, to what areas?
11) What are the expectations regarding being "on call"?
12) Will I be able to or required to work overtime?
13) Who do I talk to about time off, and what are the requirements for having it granted?
14) Who do I contact (the facility, my recruiter, my employer, other) if I have a problem or an important issue to discuss?
15) Is there an agency representative available 24 hours a day, 7 days a week?
16) What if my recruiter is unavailable?
Monday, October 30, 2006
85 million Americans CAN be wrong

A recent PEW Internet survey demonstrates that of the 80% of American Internet users who ahe searched for health information, only 25% check the source and date of the information all of most of the time. That translates to approximatel 85 million Americans whoa re "gathering health advice onlnie without consistently examining the quality indicators of the information they find. View the full PEW report here
To make sure YOU know how to evaluate health information sources on the WWW, check out some of these tools:
National Library of Medicine's Evaluating HealthInformation: a tutorial
Health on the Net (HON) Code of Conduct for medical and health Web sites
Sunday, October 29, 2006
The Children's
Well, I started my peds rotation this past Friday. I am at the Montreal Children's Hospital. Nice place, large though... long halls and I tend to get lost easily, but not as badly as when I was at the Royal Victoria last year. I was really hoping to be at the Shriner's Hospital, but hey, I am finally in peds and that is what I wanted!
The floor we are on is a real mix of cases, a medical floor. We even have one long term patient there, nice kid, lives there as he is on a vent. His room is decked out in posters/desk/computer... He goes to school in the mornings usually then comes back around 12:30-1ish. I've actually known him for nearly 18 months, as we used to take transport at the same time.
We had fun the first day on the ward. We started the day by touring the hospital and then on the ward we went on a "treasure" hunt of sorts. We were each given a scenario and had to then seek out the material and procedure info we needed in order to do it. It's fun riffling through drawers/cabinets. We then got to play with an IV pump and tubing. Everwhere we go the pump are all different so it was nice to be able to learn how to program one and trouble shoot BEFORE you actually encounter the problem on a patient.
My teacher is a doll. I love her, she is cool and fun and nice and very approachable! And she has a neat scottish accent.
My one bad aspect of this first day was that we spent from 7:30AM to 2PM walking/standing with very little break time where I could actually sit, so at the end of our conference I very nearly passed out! I felt my BP drop and I nearly dropped too. Sat down and my teacher stayed with me. I was slightly embarassed and really didn't want my teacher to see that the first day, but it gave us a chance to talk and for her to get to know me and my "needs" (ie: sit down a bit more often!).
All in all it was a good first day, I may even end up working in peds!
Thursday, October 26, 2006
Thursday, October 19, 2006
Critical Care Sedation Team

At St. Joseph Hospital, our mission is to deliver safe care and use best practices based on research and the best evidence. Implementation of a practice change is not easy, but will be successful with a dedicated and enthusiastic multidisciplinary team.
The sedation team has been meeting as a group for over one year now. We have added members and some members have left. But the goal remains clear: to develop an approach to patient centerd care of the Critical Care patient who is on the ventilator and in need of sedation. The goal of this plan was to reduce the amount of time the patient spent on the ventilator. We would accomplish this by giving the patient the best sedation at the correct levels for their individual needs. The plan included a daily awakening to assess for readiness to com off the ventilator rather than leave the patient sedated longer than necessary.
Victoria Randazzo, who is the champion of this issue as well as the chairperson of the committee, has brought together a multidisciplinary team to improve the care of this group of patients. Her team consists of Intensivist, Pharmacists, Nursing Clinical Educator, Critical Care unit management and 10 members of the nursing staff, Respiratory Department management and staff as well as Dana Rutledge, the Nurse Research Facilitator.
The team has worked together to develop a set of physician orders that adhere to the policy and procedure that Victoria authored. An education module for the critical care nursing staff was developed with input from everyone. The entire critical care staff attended the in-service which was taught completely by the nurses on the sedation team.
Following this education process, the physician orders were distributed and our plans then went into effect. In addition to this core education, one of the Intensivists provided an education seminar for the critical care staff on agitation and sedation in general. He and a sub group are working on developing a set of physician orders for the non-ventilated critical care patient.
We have just started to proceed with chart review, but we've discovered a decrease in need for patient restraints already. We expect to find fewer self-extubations and a shorter time on the ventilator with subsequent decreases in VAP as well as decreased of LOS.
We have increased patient comfort and our family survey revealed improved satisfaction when receiving care from a kind, loving nurse who is now able to efficiently reduce the agitation and maintain comfort for their loved ones while on the ventilator. The long term team effort - where all disciplines were working toward enhanced patient outcomes - increased the collegial relationship between physicians, staff nurses, respiratory therapy and pharmacy.
Wednesday, October 18, 2006
Passed
I am now waiting to get my biology test grade...
I start pediatrics tomorrow, we have 2 labs then we are in the hospital/community.
YAY!
Friday, October 13, 2006
New/updated reviews on Cochrane of interest to nurses

The following new or updated reviews from issue 3, 2006 Cochrane Library may be of special interest to nurses. To read the complete review you will need to access the subscription to the Cochrane Library. Nurses at St. Joseph Hospital,Orange and CHOC may access the Cochrane library through the library's web site.
New Reviews of special interest to nurses:
Ad libitum or demand/semi-demand feeding versus scheduled interval feeding for preterm infants
Breastfeeding or breast milk for procedural pain in neonates
Dressings for healing venous leg ulcers
Drugs for preventing postoperative nausea and vomiting
Exercise for type 2 diabetes mellitus
Routine prophylactic drugs in normal labor for reducing gastric aspiration and its effects
Updated review of special interest to nurses:
Aerobic exercise for women during pregnancy
Double gloving to reduce surgical cross infection
Fetal electrocardiogram (ECG) for fetal monitoring during labor
Mechanical devices for urinary incontinence in women
Preoperative hair removal to reduce surgical site infection
Cochrane provides free evidence summaries to support decision making during disasters

The Evidence Aid project: Resources for natural disasters and other healthcare emergencies
The following information is taken directly from the Cochrane website.
"This website highlights evidence relevant to the effects of interventions. Its aim is to help people making decisions about health care in natural disasters and other healthcare emergencies. The topics were originally identified as priorities by people in the regions affected by the 2004 tsunami, and relate to interventions that might be used or available. Where possible, a structured summary ('Evidence Update') or another summary has been prepared, based on one or more Cochrane reviews. If a summary is not available but a relevant Cochrane review exists, a link is given to the review in The Cochrane Library. If a suitable Cochrane review is not available, there are links to other sources of evidence, in particular to topics in the BMJ's Clinical Evidence. (The inclusion of links to material from outside The Cochrane Collaboration does not imply endorsement of that material by the Collaboration.) More information on Evidence Aid is available here. If you would like to comment or ask questions, please email reviews@cochrane.org. "
Infectious diseases
Injuries and wounds
Rebuilding of communities and infrastructure
Mental health
Nutrition
Rehabilitation
Thursday, October 12, 2006
Finally Over
Monday, October 9, 2006
National Institute of Nursing Research celebrates 20th Anniversary
Happy 20th anniversary National Institute of Nursing Research!! Read about the anniversary celebration.
NIH awards $700M to speed translational research at centers nationwide
 The NIH this week announced the first 12 participants in a new national consortium charged with speeding the translation of cutting-edge research into clinical practice. The grants will award 12 universities approximately $700 million over the next five years, with plans to distribute an additional $500 million to as many as 60 academic medical centers by 2012. As part of the network, centers will act as “discovery engines” that pool research data to identify scientific discoveries and apply them to real-world patient care, emphasizing improvements among underserved populations, interdisciplinary collaboration among scientists and providers, and the development of clinical informatics tools. For example, the University of California-Davis plans to use its $24.8 million grant to study chronic disease management and establish a new center for clinical and translational research, while the University of Pittsburgh will launch a patient registry program that can be tapped to identify candidates for clinical trials. The director of the NIH notes that the program marks the “first systematic change in our approach to clinical research in 50 years” (NIH release, 10/3; Neergard, AP/Yahoo! News, 10/3; Portland Business Journal, 10/3).
The NIH this week announced the first 12 participants in a new national consortium charged with speeding the translation of cutting-edge research into clinical practice. The grants will award 12 universities approximately $700 million over the next five years, with plans to distribute an additional $500 million to as many as 60 academic medical centers by 2012. As part of the network, centers will act as “discovery engines” that pool research data to identify scientific discoveries and apply them to real-world patient care, emphasizing improvements among underserved populations, interdisciplinary collaboration among scientists and providers, and the development of clinical informatics tools. For example, the University of California-Davis plans to use its $24.8 million grant to study chronic disease management and establish a new center for clinical and translational research, while the University of Pittsburgh will launch a patient registry program that can be tapped to identify candidates for clinical trials. The director of the NIH notes that the program marks the “first systematic change in our approach to clinical research in 50 years” (NIH release, 10/3; Neergard, AP/Yahoo! News, 10/3; Portland Business Journal, 10/3).Thursday, October 5, 2006
Travel Nurse: Checklist (Insurance and Benefits)
My next three posts will include a series of checklists that some of you might find helpful to utilize before taking on a new assignment. I recommend printing this and the next two posts (about checklists) out so you can have them in hand before you call or interview with your potential agencies and facilities. Here are some questions or FAQ's every travel nurse needs to ask :
INSURANCE
Ask the agency:
* Will I have insurance coverage (malpractice, life, medical, dental)?
* What are the cost and coverage for each type of insurance (maximum out-of-pocket expense, date of eligibility, premiums, and deductibles)?
* When does coverage begin for each? Who's covered? What's covered? Are existing conditions covered? If not, when will they be covered?
* Will I have a choice of health care providers and hospitals?
Can I use the insurance when I travel to other states or countries?
* Will I lose the coverage if I take a break between travel nursing contracts?
OTHER BENEFITS
Ask the agency:
* Are there other benefits and bonuses? 401(k)? Loyalty program? Continuing-education or travel reimbursement? Sign-on bonus? Completion bonus? Larger bonus for longer stay or for hard-to-fill position? Bonus for referrals?
* Does the agency offer meal allowances? Travel awards? Vacations? Special payment arrangements for items or conveniences important to me?
* If the agency pays bonuses, when would I qualify for one? What conditions must I meet to qualify for it? When would my bonus be paid? Would it be taxed?
* If the agency offers a retirement plan, when would I become eligible to contribute to it? Does the agency match my contribution? If so, when would that begin and what would the contribution consist of? When would I become vested? Into what investments would my funds be placed? Would I have control of my investments? Is there a penalty for withdrawing my money if I stop traveling?
* Will I have typical mileage reimbursement when I travel for the agency or hospital? Will the reimbursement cover a portion for transportation to the assignment and then reimbursement for return to my home (or to my next assignment)?
* Can travel reimbursement be arranged to meet my individual needs?
* How long has the travel agency been in business?
* Does the agency provide support and assistance with license processing, licensing fees, and other credentialing needs?
Asking these questions probably won’t make you the most-liked, but it will certainly help you become well-informed and better prepared. So, get out your pad and paper, and get to asking. If you conduct these simple interviews, it will assist you in deciding which agency and facility you should choose, and give you some peace of mind knowing you will be going into an assignment as a well-informed nurse.
Wednesday, October 4, 2006
Travel Nurse: My Roots In Travel
Some of my fondest memories of my youth are of family vacations. My Dad was (and still is) really into owning real estate. I think he felt like he needed to own a home in every state in the southeastern United States (and he just about did). He and my mom love to travel. When I was growing up, we had a mountain house in Tennessee. I am the one on the rock getting splashed by my sister. I love those cold mountain whitewater rivers, climbing on the slippery rocks.
Tennessee is on my list of places to spend a few months as a travel nurse. I have a looong list.
Monday, October 2, 2006
and Again...?
This time at an Amish school.
http://www.cnn.com/2006/US/10/02/amish.shooting/index.html
and possibly another near school shooting.
http://www.cnn.com/2006/US/10/02/lasvegas.schools.ap/index.html
one word: "WHY?"
Julie's picks from the Nursing Literature September

These articles caught my eye from our September 2006 current awareness search on nursing research/evidence based nursing. Staff at St. Joseph Hospital of Orange and Children's Hospital of Orange County can request copies from Burlew Medical Library or, in many cases, can obtain the full text online through the library's web site. Other individuals should contact the libraries at their institutions.
Accession Number 2009257259 NLM Unique Identifier: 16931921.Author Chulay M.Title Good research ideas for clinicians.Source AACN Advanced Critical Care. 2006 Jul-Sep; 17(3): 253-65. (20 ref)
Accession Number 2009232221 NLM Unique Identifier: 16684165.Author Ng WQ. Neill J.Title Evidence for early oral feeding of patients after elective open colorectal surgery: a literature review.Source Journal of Clinical Nursing. 2006 Jun; 15(6): 696-709. (34 ref)
Accession Number 2009172164 NLM Unique Identifier: 16620252.Author Crenshaw JT. Winslow EH.Title Actual versus instructed fasting times and associated discomforts in women having scheduled cesarean birth.Source JOGNN: Journal of Obstetric, Gynecologic, and Neonatal Nursing. 2006 Mar-Apr; 35(2): 257-64. (40 ref)
2009230807 NLM Unique Identifier: 16801357.Author Gray-Miceli DL. Strumpf NE. Johnson J. Draganescu M. Ratcliffe SJ.Title Psychometric properties of the post-fall index.Source Clinical Nursing Research. 2006 Aug; 15(3): 157-76. (30 ref)
Nursing Research. 2006 Jul; 55(4S): Supplement note: the entire supplement is on smoking cessation
2009210546 NLM Unique Identifier: 16707539.Author Dew PL.Title Is tympanic membrane thermometry the best method for recording temperature in children?Source Journal of Child Health Care. 2006 Jun; 10(2): 96-110. (56 ref)
2009237092 NLM Unique Identifier: 16825921.Author Vitale A.Title The use of selected energy touch modalities as supportive nursing interventions: are we there yet?Source Holistic Nursing Practice. 2006 Jul-Aug; 20(4): 191-6. (36 ref)
Cedars Sinai in Los Angeles: novel approach to increase handwashing

As reported in the Sept 27, 2005 Daily Briefing from the Advisory Council"
"Cedars-Sinai (Calif.): Takes novel approach to promoting hand hygiene
09/27/2006
Having exhausted traditional avenues for achieving widespread compliance with hand hygiene guidelines, Los Angeles-based Cedars-Sinai Medical Center adopted an unconventional approach to raising physician awareness and effecting behavioral change, according to a column in the New York Times Magazine. The hospital’s former chief of staff launched a widespread hand hygiene compliance effort after returning from a cruise, during which he noticed that crewmembers—who dispensed hand sanitizer during the re-boarding process and in the buffet line—were more vigilant than hospital-based providers about proper hand hygiene. Initially, Cedars-Sinai “gently cajole[d] the doctors” with faxes, e-mails, and posters advertising hand hygiene guidelines. Recognizing the need for more proactive intervention, the facility enlisted nurses to police physicians’ compliance, distributed bottles of hand sanitizer in the physician parking lot, and deployed a “Hand Hygiene Safety Posse” to award $10 Starbucks gift cards to physicians who were “caught” washing their hands. Administrators note that although these efforts raised compliance from 65% to 80%, the facility still fell short of the JCAHO-mandated 90% threshold. To take the facility’s performance to the next level, a hospital epidemiologist cultured the hands of providers involved in the hand hygiene effort and created a screensaver to be displayed on every hospital computer featuring images of the “disgusting and striking” bacteria revealed by the cultures. According to administrators, the screensavers helped push compliance to nearly 100%, a level that the facility has sustained ever since (Dubner/Levitt, 9/24). "
Saturday, September 30, 2006
Mediocre Impressions
I'm a little frustrated; I study for OB and Peds equally but have an A in one and a C in the other. I partially blame the C on the ridiculous lecture format for that course. My instructor spends the first 45 minutes of each class talking about how to study and very little time actually talking about what it is we should be studying. More often than not diseases just... aren't discussed. It's frustrating; so Meredith, Cris, and I have started making up our own chapter outlines every week in an attempt to create USABLE notes. After classes on Thursday, we just park it in the library and don't leave until we finish reviewing everything.
I miss Instructor Incredible's class. At least I learned things in there, and never felt sleepy.
My clinical experiences have been somewhat disappointing as well. I spent several days in Labor and Delivery without seeing a single birth. Then, on my LAST day there I got to witness a C-section. It was horrifying to behold because the epidural... uh... well it wasn't working. That lady was kinda screaming and fighting them. They had to hold her down in order to push general anesthesia meds... but by the time they got her under, the surgeons were already cutting through the uterus. I observed all this while pressed up against the back wall with several other speechless students. Apparently this was a very unusual occurrence, but since it was the only live birth I've ever seen, my perceptions of the process will forever be skewed. This has only confirmed my extreme distaste for labor-type nursing.
Peds is disappointing mostly because I am being held on such a short leash. We aren't even giving meds! I understand the caution with which one must treat kids... but I feel like too much of my time is spent sitting idly by rather than providing care. Also, my patience with children is fairly thin, but my patience with parents is even less substantial.
In short, I'm not having the fabulous time I was used to having. That's probably more my fault than anyone else's. Therefore I'm going to have to work especially hard at observing Instructor Exhausted and Instructor Technology if I'm going to uncover the gems of wisdom I previously found so abundant. In the meantime, I look to my Nurse Tech job as a source of inspiration.
Procrastinating...

I should be studying for a nursing class test and a bio quiz and working on my nursing care plan, but instead I am reading email and forwarding funny jokes, so here is one of my favorites:
It doesn't hurt to take a hard look at yourself from time to time,
and this should help get you started
During a visit to the mental asylum, a visitor asked the Director
what the criterion was which defined whether or not a patient
should be institutionalized.
"Well," said the Director, "we fill up a bathtub, then we offer a
teaspoon, a teacup and a bucket to the patient and ask him or her
to empty the bathtub."
"Oh, I understand," said the visitor. "A normal person would use
the bucket because it's bigger than the spoon or the teacup."
"No." said the Director,
"A normal person would pull the plug. Do you want
a bed near the window?"
DID YOU PASS, OR DO YOU WANT THE BED NEXT TO MINE ?
Wednesday, September 27, 2006
Again?
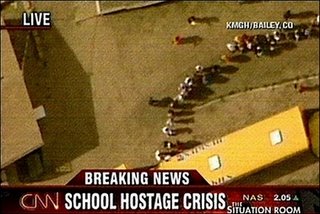
And so it happened again. A shooter entered a school in Colorado and shot and killed a female student, then took his own life after holding 6 girls hostage for 4 hours.
There are no words left to say... sadness is what I feel.
When will this type of stupidity end?
http://news.yahoo.com/s/ap/20060928/ap_on_re_us/school_evacuation
Monday, September 25, 2006
Travel Nurse: Have Husband, Will Travel
 You don't have to be single to be a traveling nurse.
You don't have to be single to be a traveling nurse.While most travel nurses are single, my experience has been that there are also a large number of nurses that travel with their husbands. The majority of them that travel around do find some sort of work in the location the nurse is working in.
Some have "portable" jobs like an online or internet business, or a "work-from-home" type job. Others have been able to find short-term positions, that they arrange prior to relocating, that only last for the duration of the contract.
Your spouse could also explore working in the hospital you will be in. The demand for nurses is so great, that they may be willing to employ your spouse just to get you to their facility. Consider speaking to your travel nursing recruiter about negotiating this before you sign to work at any hospital. Many hospitals are glad to accomodate you and, depending on their needs, are happy to gain two new employees rather than one.
It is easy to find work in a majority of the areas you travel in, but if you are looking to relocate to be at travel nurse in a rural community, it may be difficult to find jobs for your spouse. In those types of isolated conditions there aren't usually many job availablilties, but if the pay is good enough to sustain both of you, then your husband could consider being a "house husband," which usually works out great, especially if he's a dad too.
If your husband finds it difficult to find a job that will allow only temporary employment, remember-you can always renew your assignment contract and stay for an extended period and if you end up liking the location, you can always take on a permanent position at the hospital there.
Sunday, September 24, 2006
Cold Case...
Friday, September 22, 2006
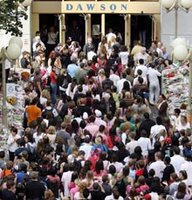
And so we move on

On Friday, September 22, students and staff met at 11:00 a.m. at the de Maisonneuve entrance to remove the flowers together. They were placed on the West grounds and will be made into compost for a garden to be planted in the future. Thank you to all who participated.
Thank you Dawson for doing this. We need to move on and this was the perfect way of doing so.
Wednesday, September 20, 2006
WOW! I feel like a "real" nurse!
One Week Later



Last Wednesday we, Dawson College students, staff, faculty and friends, were frightened and lost. We went through a terrible ordeal, one young life lost and 20 others injured, 2 still remain in coma.
I thank all who support us still, friends, family, teachers/staff.
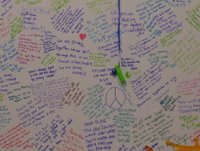
Todays blog is about that. I want to show others what the school has done for us, to help us get through this as a "family".
One pic is of the doors with messages taped onto them, one is of all the flowers that have been left,(and this is just a small sampling of what is around the school), one is one the "cafeteria" wall where it all hapened, it has big white boards that we were able to write messages, and one is a close up of my message "Let us unite and be strong, show others who we are"
Monday, September 18, 2006
Today we stood as one

Today was tough... real tough. The school did an amazing job at welcoming us back though. Staff/teachers/psychologists all were there to greet us outside and inside the school. They clapped and said welcome back, we are glad you came. Teachers who don't even know you would walk up to you and ask if you are ok.
I went to the nursing dept. and spoke to my teachers and hung out with friends. We cried and lauged, we ate (there was tons of food). We then went to the main cafeteria and signed the books they had set up, full of messages from us, the student body. We signed the "wall", large poster boards were hung with markers and we could write whatever we wanted.
So the first day back is over and I find myself still crying when I stop and think about all that has happened, but I know that I have friends and teachers who are there for me, no matter what.
Thank you to all who support Dawson College and all of it's students. Montrealers have shown us that they love us, they support us and feel the same sadness we felt on that day and the days since.
Sunday, September 17, 2006
Normal?

Nothing will feel normal tomorrow.
Sure there won't be signs of the bloody violence that occured in my school, at least not any physical signs to the inside of the building... blood, bullets, all gone. But the memories are there, the feelings we have are there and the remaing fear is there too.
They say (psychologists and the like) that for 95% of us, this fear and sadness will decrease and disapear in the next 2 weeks. But what about the remaining 5% ? Those who SAW it ALL happen? Like my friend M who watched in horror as the gunman shot and killed one and shot 19 others.
I'm not sure when "normal" will return, or if it ever really will. Dawson is a great place with great people. The support that has been shown our "community" has been amazing. Our teachers have been and will be supportive and comforting. There are many activities set up for us tomorrow in many dept. as well as for the school in general.
Life goes on, it has to. For me it always has, no matter what the challenge... this is yet another one I have to face.
Friday, September 15, 2006
Jean Watson's theory selected as framework at St. Joseph Hospital, Orange, California
Additionally, we will be offering a special viewing of a moving and inspirational DVD on the "Theory of Human Caring" which was produced by SJH nurses.
One hour sessions are scheduled in the Zhoul auditorium on
Monday Sept 18 12:00 noon to 1:00 pm 2006
Tuesday Sept 19 7:30 am - 8:30 am
Tuesday Oct 3 7:30 - 8:30 am
Monday Oct 16 12:00 noon to 1:00 pm
Friday Nov 3 7:30 am - 8:30 am
Monday Nov 6 12:00 noon -1:00 pm
No registration is required and breakfast/lunch will be served to St. Joseph Hospital of Orange staff.
Along these same lines, there is a very cool Nursing Theory Link page out of Clayton State University Department of Nursing where you can read about many nursing theories.
Evidence Based Library Science Conference

Evidence Based Library & Information Practice4th International Conference"Transforming the Profession"May 6-11, 2007, Chapel Hill-Durham, North Carolina, USA http://www.eblip4.unc.edu/ The Evidence Based Library and Information Practice Conference(EBLIP4) is an exciting international event that has emerged inresponse to the growing interest among all types of libraries in usingthe best available evidence to improve information practice. The conference on May 6-9, 2007 in Chapel Hill, North Carolina will be followed by two days of continuing education. The conference provides a forum for the presentation of high quality papers and posters aswell as examples of how EBLIP is being implemented in library and information settings around the globe. EBLIP4 invites submissions for contributed papers and posters including both original research and innovative applications of EBLIP in library and information management. Papers that deal with library support of evidence-based practice in other fields such as health, social work and public policy are also welcome.
Full instructions to authors may be found at http://www.eblip4.unc.edu/ Chapel Hill-Durham is located in the middle of the Eastern United States close to the Raleigh-Durham international airport. This central location in the Research Triangle area is only a short drive from scenic locations in North Carolina. The beaches are approximately two hours to the east and the mountains are two hours to the west. Washington DC is a 4.5 hour drive or 30 minutes by air. Important Dates
December 1, 2006 Submission deadline for abstracts for papers and posters
February 11, 2007 Final decisions for accepted papers
February 15, 2007 Final decisions for accepted posters
March 15, 2007 Submission deadline for full papers
Carol Perryman MSLISTRLN Doctoral FellowSchool of Information & Library ScienceUniversity of North Carolina at Chapel Hill
Thursday, September 14, 2006
...Update
2 people remain in comas, one sedated on purpose to be in a coma, the other not. Very sad. 4 are left in the ICU still, including these 2 in comas.
Wednesday, September 13, 2006
Shooting at MY school...?
2 people are in critical condition on life support from what we've heard.
It was and is still, very frightening. I cannot believe this happened at MY school. You always hear about these things, but you never think it could be your school.
Again I wonder, What is this world coming to?
Advertise on this Blog
Thank you,
Amy Robbins
Monday, September 11, 2006
Back to School!
I'm a little pissed off because I'm having to take a statistics class. It's not so bad by itself, but I already took Stat as a math class in Houston. But does the school want that credit? Noooo, they want Psychology Statistics. I've fought and pleaded. I've asked to take a test, but to no avail! Basically I'm paying them money to sit around and re-learn things I've already mastered. On top of that, I find that many nurses are none-to-bright about math, and the pace of study is agonizingly slow compared to the first go-round. Let's hope I don't go crazy. ^_^;;
I'm still working as a tech in the PCU. I'd never really considered PCU as a place to start a nursing career, but it's becoming more appealing all the time. First of all, the patient ratio is lower than Med-Surg, but the patients aren't quite as critical as in the ICU. Secondly, the hospital is interested in "cross-training" people in ICU and ER skills in order to provide more options for "floating" extra staff in times of low census. Thirdly, I like the floor I'm on, and wouldn't mind working with these people in a larger capacity.
I've always been far more interested in critical care than anything else, mostly because I'm not too fond of children or surgery or the like. And I want to be in a place that will challenge me and keep me on my toes. Still keeping my options open, but it looks like this hospital has accomplished it's own goals by recruiting me for this job: getting me comfortable with this facility and reeling me in for employment after graduation.
We'll see how things work out when I graduate. If I don't end up in Texas, I really hope I end up right where I am.
Tomorrow I'm going to spend clinicals in Labor and Delivery. I reaallly hope a baby is born in the time that I am there, because I feel like that would be much more exciting than just hanging out with a woman moaning in labor for 8 hours. o_O
Taken two tests sofar. I actually made an A on the second one! (I'd almost forgotten how it felt to make A's on big tests with this funky grading scale!) My extra preparation is paying off. I'm making time to read the chapters before lecture and staying at least 2 hours afterwards in the library for review. And that works. (Well... except when a question is vague or weird. But that's not my problem.)
I really really want to do well this semester so I can increase those decimals after the 3 in my nursing gpa. I want to be inducted into Sigma Theta Tau! They only take the upper percent of the class, so I don't know what my chances are. If I keep making As though, maybe they'll improve. ^_^
Friday, September 8, 2006
Study: Nurses Lack IT training

A new study in eWeek finds that most nurses receive minimal or no IT training. Information literacy is integral to an understanding of how to approach Evidence Based Nursing.
Please post your comments below if you have any great ideas/suggestions on this topic.
Resources for teaching EBM
Thursday, September 7, 2006
Travel Nurse: Earn Money While Visiting With Family

When my husband and I got married we decided we wanted to live near extended family so we (and our children) could remain close to them. The only problem was that my parents lived in Georgia, and his lived in Utah… so we had to pick. We chose Georgia.
After our son turned one, we decided we wanted to spend some time “out west” to let him get to know his grandparents, aunts, uncles, and cousins that live out there better, and to enjoy the sites. We didn’t have a whole lot of money with my husband in school so we knew that one of us would have to work if we wanted to stay for the whole summer.
That is where travel nursing helped out. My husband was not going to be in school for the summer, so we planned for him to stay home with our son while I worked. Most of the hospitals there wanted me to work three twelve hour shifts per week (which is what I preferred anyways). I had the choice of working either an 8 or 12 week assignment. We chose the 8 week one so we could have one month off to vacation. There were so many things to do out there that we enjoy (i.e. hiking, camping, rafting, and biking). All our travel (relocation) expenses were reimbursed (tax-free). We received a monthly housing stipend which was just an added bonus since we stayed with family. We ended-up making $12,080 in two months! Now try and beat that for a career! Now that my son is almost five, we often reflect back on that summer in Utah. What a great time we had, and how grateful I am that I chose nursing as a career.
Wednesday, September 6, 2006
Pressure Ulcers among Eldery Patients Early in Hospital Stay: Abstract with commentary by Dana Rutledge, RN, PhD
Background. Pressure ulcers among elderly hospital patients diminish quality of life and increase the cost of hospital care. Evidence suggests that pressure ulcers can arise after only a few hours of immobility. The goals of this study were to estimate the incidence of hospital-acquired pressure ulcers in the first 2 days of the hospital stay and to identify patient characteristics associated with higher incidence.
Methods. A prospective cohort study was performed between 1998 and 2001. A total of 3233 patients 65 years old or older admitted through the Emergency Department to the inpatient Medical Services at two study hospitals were examined by a research nurse on the third day of hospitalization. Pressure ulcers were ascertained using standard criteria and were classified a either preexisting, possibly hospital-acquired, or definitely hospital-acquired.
Results. There were 201 patients with one or more possibly or definitely hospital-acquired pressure ulcers for a cumulative incidence of 6.25 (95% confidence interval, 5.4% - 7.1%). Most of the pressure ulcers were stage 2, and the majority were in the sacral area or on the heels. In multivariable analysis, pressure ulcer incidence was significantly associated with increasing age, male gender, dry skin, urinary and fecal incontinence, difficulty turning in bed, nursing home residence prior to admission, recent hospitalization, and poor nutritional status.
Conclusions. A small but significant proportion of elderly emergently admitted hospital patients acquire pressure ulcers soon after their admission. New models of care may be required to ensure that preventive interventions are provided very early in the elderly person’s hospital stay.
Baumgarten, M. et al. (2006). Pressure ulcers among elderly patients early in hospital stay. Journal of Gerontology: MEDICAL SCIENCES, 61A, 749-754.
Commentary by Dana N. Rutledge, RN, PhD, Nursing Research Facilitator
Were you surprised at any of the predictors of pressure ulcers in this hospitalized elderly patients? You probably were not. Studies using the Braden Pressure Ulcer Risk Assessment Scale confirm that problems with moisture, mobility/activity, and nutrition are all predictors of pressure ulcer development. What is new about the Baumgarten et al. study is that in 6.2% of the patients, pressure ulcers developed within 3 days of hospital admission!! Earlier studies have not specifically looked at this time interval.
What were the strengths and limitations of the study. Strengths include the large sample size, use of 2 hospitals (one in Pennsylvania, one in Oregon), the large sample of African Americans, and use of trained research nurses to evaluate the study measures. Limitations are that the study involved only a brief one-time observation of the patients and that hospital-acquired and preexisting pressure ulcers may have been somewhat misclassified.
Taking these into account, what is the take home message for the practicing nurse? Elderly patients admitted to medical units may be prone to develop pressure ulcers within 3 days of admission. Thus, given recent trends towards shorter hospital stays, the potential for breakdown is high. Nurses MUST put preventive measures into place early!!
Tuesday, September 5, 2006
toe update
Friday, September 1, 2006
Trip database-- free access

Trip Database :Turning Research into Practice
For the last 4 years, the Trip database has been a subscription service, but as of Sept 2006, it is once again a free resource. TRIP describes itself as " the Internet's leading resource for Evidence-Based Medicine allowing users to easily and rapidly identify the highest quality evidence from a wide range of sources." This site has recently been evaluated by a team from the Centre for Evidence-Based Medicine. Although not nursing focused, this free resource is a great one-stop source for answering clinical questions. The site supports Boolean searching and returns results that you can then filter by such entities as : evidence based synopses, clinical questions, systematic reviews, guidelines, e-textbooks, clinical calculators and even by medical speciality. You can also sign up for the Trip Blog on their web site.
Evidence Based Nursing Blog "Down Under"
A Nursing Evidence Based Practice Tutorial
Our blog discussed in Evidence Soup blog
Julie's August picks from the literature

Some of these recent articles really intrigued me. Employees at St. Joseph Hospital, Orange or Children's Hospital of Orange County can access these online or request them through Burlew Medical Library. Others should consult medical libraries with whom they have privileges.
Accession Number 2009223633 NLM Unique Identifier: 16816597.Author Coopey M. Nix MP. Clancy CM.Title Translating research into evidence-based nursing practice and evaluating effectiveness.Source Journal of Nursing Care Quality. 2006 Jul; 21(3): 195-202. (9 ref)
Accession Number 2009232462 NLM Unique Identifier: 16767023.Author Giuliano KK.Title Continuous physiologic monitoring and the identification of sepsis: what is the evidence supporting current clinical practice?Source AACN Advanced Critical Care. 2006 Apr-Jun; 17(2): 215-23. (36 ref)
Accession Number 2009232451 NLM Unique Identifier: 16767019.Author Albert NM.Title Evidence-based nursing care for patients with heart failure.Source AACN Advanced Critical Care. 2006 Apr-Jun; 17(2): 170-85. (41 ref)
Accession Number 2009211028 NLM Unique Identifier: 16766627.Author Munro CL. Grap MJ. Jablonski R. Boyle A.Title Oral health measurement in nursing research: state of the science.Source Biological Research for Nursing. 2006 Jul; 8(1): 35-42. (47 ref)
Tuesday, August 29, 2006
Travel Nurse: Four Reasons to Consider Travel Nursing
 I found this picture of a lady lounging around in a hammock and decided to put it in a post because that is one of mis pasatiempos favoritos (to recall one of the only phrases I remember from Spanish I in high school). The main reason I decided to become a travel nurse was the opportunity to see new places and experience new things. But there are certainly other reasons to consider travel nursing.
I found this picture of a lady lounging around in a hammock and decided to put it in a post because that is one of mis pasatiempos favoritos (to recall one of the only phrases I remember from Spanish I in high school). The main reason I decided to become a travel nurse was the opportunity to see new places and experience new things. But there are certainly other reasons to consider travel nursing.Reason No. 2
Travel nursing has given me an opportunity to see how different facilities work in different parts of the United States. Most of the facilities I have worked in have been hospitals. I have noticed that many of the hospitals I have worked in are primarily about the "bottom line." How many patients can we put in how many beds to turn a profit? I would go to work like every other nurse, do my job and go home. Not much fun. However, I have worked in one hospital that was clearly more concerned about patient care and employee well being than turning a profit. At least that is how it seemed to me. Employees had access to onsite recreation facilities and patients had large, well furnished rooms and "gourmet" meals. If and when I decide to take another assignment in St. Louis that is the facility I would want to work in again.
Reason No. 3
Higher pay. I know that it is kinda' taboo to discuss pay at work, but everywhere I have worked it doesn't take long for me to find out how much everyone is making. Usually lunchtime conversation. It has been my experience that I make on average $10.00 to $20.00 more than regular nurses because I am a travel nurse.
Reason No. 4
If the job stinks, I usually only have to endure it for 3 months. And, if it is too bad, I just need to request that my agency find someone to replace me. I have not had to do this yet, but I have been told that it usually doesn't take very long.






