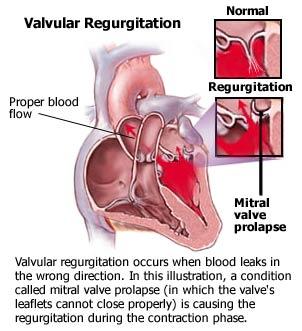
Mitral insufficiency causes an increase in blood volume in both the left atrium and ventricle. This situation occurs because of the regurgitant blood that flows from left atrium to left ventricle to left atrium again. The increased volume of blood in chronic mitral insufficiency accumulates slowly, allowing the left atrium and left ventricle to increase in size. The heart, therefore, tolerates the regurgitant blood flow without engorgement of the pulmonary circulation or reduction of cardiac output. In acute mitral insufficiency, the left atrium and ventricle are not able to tolerate the dramatic increase in blood volume, so cardiac output decreases and blood backs up quickly into the pulmonary circulation. Pulmonary congestion and acute illness follow.
Nursing care plan assessment and physical examination
Question the patient about a history of rheumatic fever because 50% of all cases of chronic mitral insufficiency are attributed to rheumatic heart disease. Because mitral valve prolapse, a common form of mitral insufficiency, has a familial association, determine if others in the family have the condition. Coronary heart disease contributes to both chronic and acute disorders; therefore, ask the patient if she or he has chest pain or palpitations. Determine if the patient has the classic symptoms of fatigue and shortness of breath. Other symptoms include orthopnea, palpitations, irregular heartbeat, exertional dyspnea, edema, and weight loss.
Inspection and palpation of the precordium are usually unremarkable except in extreme cases of mitral insufficiency. Auscultation of the chest usually reveals a soft first heart sound and a systolic murmur, which is loudest at the apex. In severe mitral insufficiency, you may hear an S3 gallop. Auscultation of breathing may reveal fine crackles (rales) if pulmonary congestion is present. When the abdomen is palpated, you may note an enlarged liver if the patient has severe right-sided heart failure. The patient may also have jugular vein distension and a prominent alpha wave.
In an effort to avoid exertional dyspnea and fatigue, patients usually adjust their lifestyles by restricting their activity and resting frequently. They may not notice the increasing fatigue until it gets debilitating. Assess the patient’s level of exercise and how he or she copes with activity intolerance.
Nursing care plan primary nursing diagnosis: Activity intolerance related to diminished cardiac output.
Nursing care plan intervention and treatment plan
Physicians place most patients with advanced mitral insufficiency on activity restrictions to decrease cardiac workload. Research suggests that if the patient is on bedrest, the use of a bedside commode creates less workload for the heart than using a bedpan. Fluid restrictions and diuretics may be ordered to reduce pulmonary congestion. Supplemental oxygen enhances gas exchange and oxygenation to decrease dyspnea and chest pain.
Most patients with mitral insufficiency can compensate or be stabilized with medical treatment for their entire lives. Surgical repair or valve replacement is considered in patients with progressive severe disease. Mitral valve repair (valvuloplasty) is preferred over replacement whenever possible. The choice of valve type is based on the patient’s age and the potential for clotting problems. A biologic valve (such as a porcine valve from a pig) usually shows structural deterioration after 6 to 10 years and needs to be replaced. A synthetic valve is more durable but is also more prone to thrombi formation. If the incompetent valve is replaced surgically with a synthetic valve, patients are prescribed long-term anticoagulant therapy, such as warfarin (Coumadin).
Maintain airway, breathing, and circulation. If the patient is stable, focus on reducing the cardiac workload and psychological stress to reduce the metabolic demands of the myocardium. Provide assistance with activities of daily living, and encourage the patient to abide by activity restrictions to allow for adequate rest. Establish a quiet environment with uninterrupted rest periods, if possible. To ease the patient’s breathing, elevate the head of the bed. Encourage the patient to avoid sudden changes in position to minimize increased cardiac demand and dizziness. Instruct the patient to sit on the edge of the bed before standing.
Reduce psychological stress by approaching the patient and family in a calm, relaxed manner. Decrease fear of the unknown by providing explanations and encouraging questions. Help the patient maintain or reestablish a sense of control by participating in decisions about aspects of care. If the patient decides to have valve surgery, offer to let the patient speak with someone who already has had the surgery.
Nursing care plan discharge and home health care guidelines
Be sure the patient understands all medications, including the dosage, route, action, and adverse effects, and the need for routine laboratory monitoring for anticoagulants. Explain the need to avoid activities that may predispose the patient to excessive bleeding; hold pressure on bleeding sites to assist in clotting. Remind the patient to notify healthcare workers of anticoagulant use before procedures. Identify foods high in vitamin K, such as turnips, spinach, liver, and cauliflower, which should be limited so the effect of warfarin is not reversed. Instruct the patient to report the recurrence or escalation of signs and symptoms of mitral insufficiency. The appearance of these symptoms could indicate that the medical therapy needs readjusting or that the replaced valve is malfunctioning. Patients with synthetic valves may hear an audible click from the valve closure. The click sounds like the ticking of a watch.
Patients who have had valvular disorders or valve surgery are susceptible to bacterial endocarditis, which causes scarring or destruction of the heart valves. Bacterial endocarditis may result from dental work, surgeries, and invasive procedures, so people who have repaired or replaced heart valves should be given antibiotics before and after these treatments.
No comments:
Post a Comment