Of the more than 60,000 new cases of lymphoma that are diagnosed each year in the United States, approximately 55,000 of them will be NHL. In the past 30 years, the incidence of NHL has increased by more than 80%, making it one of the largest increases of any cancer. This increase is unexpected and is only partially explained by earlier detection because of improved diagnostic techniques or human immunodeficiency virus (HIV)–associated lymphomas.
Malignant lymphoma, or NHL, is a heterogeneous grouping of several disease types that range from the aggressive, rapidly fatal diffuse histiocytic lymphoma to the indolent nodular varieties. Still, all have a less promising prognosis than Hodgkin’s disease. Complications of NHL include hypercalcemia, increased uric acid levels, meningitis, and anemia. As tumors grow, they may compress the vital organs and cause organ dysfunction; problems from organ compression include complications such as increased intracranial pressure.
Nursing care plan assessment and physical examination
Note any history of infection with HIV, acquired immunodeficiency syndrome (AIDS), organ transplant, congenital immunodeficiency, autioimmune diseases, or other treatment with immunosuppressive drugs. Patients often have complaints of painless enlarged lymph nodes (commonly in the neck, mediastinum, or chest wall), fevers, night sweats, weight loss, weakness, and malaise. Because nodes and extranodal sites are more likely to be involved in NHL, the patient may also report vague abdominal distress (bleeding, bowel obstruction, cramping, ascites), symptoms of spinal cord compression, or back pain. Cough, dyspnea, and chest pain occur about 20% of the time and are indicative of lung involvement.
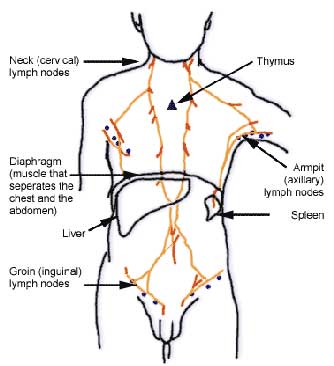
Carefully inspect all the locations for lymph nodes and the abdomen for signs of hepatosplenomegaly and ascites. Skin lesions that look like nodules or papules with a tendency to ulcerate appear in about 20% of cases. When palpating lymph node chains, examine the submental, infraclavicular, epitrochlear, iliac, femoral, and popliteal nodes. Involved nodes are characteristically painless, firm, and rubbery in consistency; they are in contrast to the rock-hard nodes of carcinoma because they are freely movable and of varying size. Palpate the liver or spleen, which may be enlarged. The patient may also have weight loss and fever.
The diagnosis of cancer is devastating at any time of life. Because the disease is most common in the older adult, the patient may be planning retirement. The diagnosis of NHL throws all retirement plans into disarray and may lead to feelings of loss, grief, and anger.
Nursing care plan primary nursing diagnosis: Risk for infection related to impaired primary and secondary defenses.
Nursing care plan intervention and treatment plan
Treatment is based on classification of the cell and staging of the disease. Some of the indolent types of NHL do well with only supportive therapy. The disease process may be slow enough that treatment is saved until the disease takes a more aggressive path. Most patients with intermediate- grade and high-grade lymphomas receive combination chemotherapy. Radiation is effective for many patients with stage I or II NHL. Radiation is delivered to the chest wall, mediastinum, axilla, and neck (the region known as the mantle field). Most patients, however, are at stage III or IV at diagnosis. Surgery has limited use in the treatment of NHL. It may be part of the diagnostic and staging process, but diagnostic laparotomy is much less common than in Hodgkin’s disease. A therapeutic splenectomy may be performed for severe spleen enlargement. Gastric or bowel resection may be done if the patient has a primary gastrointestinal lymphoma or has obstructions from bulky nodes. Stem cell transplantation may be considered for patients who have relapsed, are at high risk for relapse, or have tried conventional therapy without success.
Maintain the patient’s comfort, protect the patient from infection, provide teaching and support about the complications of the treatment, and provide emotional support. Fatigue, one of the most common side effects of cancer treatment, can last for several months to several years. A program entitled “Fatigue Initiative Research and Education” (FIRE) is available through the Oncology Nurses Society (www.ons.org).
During irradiation, the patient may suffer from dry mouth, loss of taste, dysphagia, nausea, and vomiting, which can be managed with frequent mouth care. Explore ways to limit discomfort, such as ice chips. Attempt to provide desired foods to support the patient’s nutrition. Keep any foul-smelling odors clear of the patient’s environment, particularly during meals. Manage skin irritation and redness by washing the skin gently with mild soap, rinsing with warm water, and patting the skin dry. Encourage the patient to avoid applying lotions, perfumes, deodorants, and powder to the treatment area. Explain that the patient needs to protect the skin from sunlight and extreme cold. Before starting treatments, arrange for the patient to have a wig, scarf, or hat to cover any hair loss, which occurs primarily at the nape of the neck.
If the patient develops bone marrow suppression, institute infection controls. Treat the discomfort that may arise from chemotherapy—joint pain, fever, fluid retention, and a labile emotion state (euphoria or depression)—all of which need specific interventions, depending on their incidence and severity. The complexity of the diagnostic and staging process may make the patient feel lost in a crowd of specialists. It is important for the nurse to provide supportive continuity. Patience and repeated explanations are needed. Provide the patient with information about support groups, and refer the patient to a clinical nurse specialist, support groups associated with the American Cancer Society (www.cancer.org), or counselors.
Nursing care plan discharge and home health care guidelines
Teach the patient the following strategies to limit infections: avoid crowds, avoid infected visitors, particularly children with colds, wash the hands frequently; when an infection occurs, report it to a physician immediately; avoid direct contact with pets to limit the risk of infections from licks, scratches, or bites; do not change the cat litter or clean a birdcage. Maintain a high-calorie and high-protein diet. Take sips of grapefruit juice, orange juice, or ginger ale if nausea persists. Drink at least 2000 mL of fluid a day unless on fluid restriction. Perform frequent mouth care with a soft toothbrush and avoid commercial mouthwashes. Contact support groups, the American or Canadian Cancer Society, or counselors as needed.
No comments:
Post a Comment