Normally, the placenta implants in the body (upper portion) of the uterus. Implantation allows for delivery of the infant before the delivery of the placenta. With placenta previa, the placenta is implanted in the lower uterine segment over or near the internal os of the cervix. As the uterus contracts and the cervix begins to efface and dilate, the villi of the placenta begin to tear away from the uterine wall and bright red, painless, vaginal bleeding occurs. The bleeding is facilitated by the poor ability of the myometrial fibers of the lower uterine segment to contract and constrict the torn vessels. Bleeding can occur antepartally or intrapartally. Hemorrhage from the placental site may continue into the postpartum period because the lower uterine segment contracts poorly, contrasted with the fundus and body of the uterus. Placenta previa is classified in four ways, depending on the degree of placental encroachment on the cervical os. The degree of the previa depends largely on the cervical dilation. For example, a marginal previa at 2 cm may become a partial previa at 8 cm because the dilating cervix uncovers the placenta. Sometimes, a placenta may correct itself, especially if it low-lying; as the uterus enlarges, the placenta moves cephalad. Depending on the amount of blood loss and gestational age of the fetus, placenta previa may be life-threatening to both the mother and the fetus.
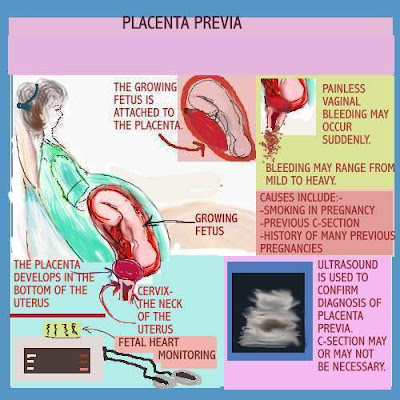
The cause of placenta previa is unknown, but it is more common in women who have a history of uterine surgeries (cesarean sections, dilation and curettage), infections with endometritis, and a previous placenta previa. It is also more common in those women who currently have a multiple gestation with a large placenta. Smoking is also a contributing factor.
Nursing care plan assessment and physical examination
Although many women who develop placenta previa have an unremarkable obstetric or gynecologic history, some have had previous uterine surgeries or infections. The prenatal course of the current pregnancy is often uneventful until the patient experiences a bout of bright red, painless bleeding. Question the patient as to the onset and amount of bleeding first noticed. The initial bleeding in placenta previa is often scant because few uterine sinuses are exposed.
The classic sign of placenta previa is painless, bright red bleeding; assess the amount and character of blood loss. Most often this bleeding occurs between 28 and 34 weeks when the lower uterine segment thins and the low implantation site is disrupted. With a marginal or low-lying placenta previa, the bleeding may not start until the patient is in labor. Assess the uterus for contractions; unless the patient is in labor, the uterus is relaxed and nontender. A vaginal examination should not be performed because even the gentlest examination can cause immediate hemorrhage.
Check the vital signs; note any symptoms of hypovolemic shock (restlessness; agitation; increased pulse; delayed capillary blanching; increased respirations; pallor; cool, clammy skin; hypotension; and oliguria). Monitor the baseline fetal heart rate and the presence or absence of accelerations, decelerations, and variability in the electronic fetal monitoring (EFM).
Ask the patient if she feels the fetus move. Assess the fetal position and presentation by using Leopold’s maneuvers. Monitor the patient’s contraction status, and palpate the fundus to determine the intensity of contractions. View the fetal monitor strip to assess the frequency and duration of the contractions; more often, the uterus is soft and nontender, unless the patient is in labor. Throughout the patient’s hospitalization, continue to monitor for signs of hypovolemic shock and the amount and character of bleeding. Maintain continuous EFM until bleeding ceases; then, if hospital policy permits, monitor the fetus for 30 minutes every 4 hours.
The heavy, bright red bleeding that often accompanies placenta previa is anxiety producing for the mother and significant others. The patient is concerned not only for herself but also for the well-being of the infant. Determine the patient’s support system because many of these patients have been on complete bedrest for an extended period of time. Assess the effect of prolonged bedrest on the patient’s job, childcare, interpersonal, financial, and social responsibilities.
Nursing care plan primary nursing diagnosis: Fluid volume deficit related to blood loss.
Nursing care plan intervention and treatment plan
Management of a patient with placenta previa depends on the admission status of the mother and the fetus, the amount of blood loss, the likelihood that the bleeding will subside on its own, and the gestational age of the fetus. If both the mother and the fetus are stable and the fetus is immature (less than 37 weeks), delivery may be put off and an intravenous (IV) infusion started with lactated Ringer’s solution. In addition, the patient is maintained on bedrest with continuous EFM. Closely monitor the fetal heart rate. If any signs of fetal distress are noted (flat variability, late decelerations, bradycardia, tachycardia), turn the patient to her left side, increase the rate of IV infusion, administer oxygen via face mask at 10 L/min, and notify the physician. Once the bleeding has ceased for 24 to 48 hours, the patient may be discharged to her home on bedrest before delivery. This conservative treatment gives the preterm fetus time to mature. If the patient is in labor and a marginal placenta previa is present, the physician allows her to labor and deliver vaginally, with careful surveillance of maternal and fetal status throughout the labor. Postpartum, the patient will require oxytocics to prevent hemorrhaging, owing to the poor ability of the lower uterine segment to contract.
If fetal distress is present or if the patient has lost a significant amount of blood, an immediate cesarean section and, possibly, blood transfusions are indicated. If the patient delivers (vaginally or by cesarean), monitor her for postpartum hemorrhage because contraction of the lower uterine segment is sometimes not effective in compressing the uterine vessels that are exposed at the placental site. Although medication is not given to treat a previa, pharmacologic treatment may be indicated to stop preterm labor (if it is occurring and if bleeding is under control), enhance fetal lung maturity if delivery is expected prematurely, or prevent Rh disease, if the patient delivers.
If the patient is actively bleeding, and mother and fetus are stable, maintain the patient on bedrest in the lateral position (preferably left lateral) to maximize venous return and placental perfusion. Because the patient may be on bedrest for an extended period of time, comfort can be increased with back rubs and positioning with pillows. Provide diversional activities and emotional support. The nurse should make every attempt to explain the condition, treatment, and potential outcomes to the patient. Often, if a preterm delivery is unavoidable, a special care nursery nurse comes in and discusses what the mother can expect to happen to her infant on admission to the neonatal intensive care unit.
Nursing care plan discharge and home health care guidelines
If the patient is discharged undelivered, provide the following instructions: Notify the physician of any vaginal bleeding, spontaneous rupture of membranes, decreased fetal movement, or regular labor contractions. Maintain continuous bedrest with bathroom privileges. Avoid the supine position; use the lateral or semi-Fowler position. Abstain from sexual intercourse.
Be sure to have the means to reach the hospital at all times.
No comments:
Post a Comment