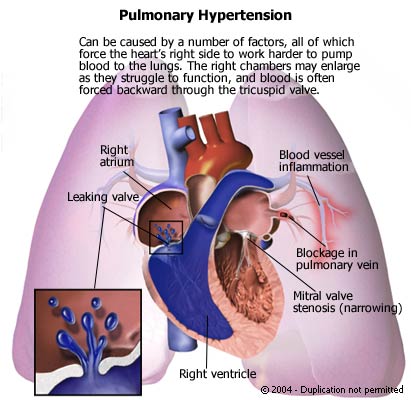
Pulmonary hypertension is diagnosed when the systolic pressure in the pulmonary artery exceeds 30 mm Hg. It is most commonly seen in preexisting pulmonary or cardiac disease but may occur (although rarely) as a primary condition when it is produced by fibrosis and thickening of the vessel intima. An increase in resistance of the vessels in the pulmonary vasculature bed occurs secondary to hypoxemia (oxygen deficiency). Chronic hypoxemia produces hypertrophyof the medial muscle layer in the smaller branches of the pulmonary artery, which decreases the size of the vessel lumen. Vasoconstriction, the pulmonary system’s response to hypoxemia, results in a pressure buildup in the right side of the heart because flow through the pulmonary system is impaired. When hypertension in the pulmonary system (measured as pulmonary vascular resistance) is greater than the ability of the right side of the heart to pump, the cardiac output falls and may cause shock.
The cause of primary pulmonary hypertension is unknown, but the disease tends to occur in families. Secondary pulmonary hypertension is caused by conditions that produce hypoxemia, such as chronic obstructive pulmonary disease, obesity, alveolar hypoventilation, smoke inhalation, and high altitude.
Nursing care plan assessment and physical examination
Patients are usually without symptoms until late in the disease. Up to 50% of the pulmonary circulation may be impaired before significant hypertension is produced. Determine the presence of risk factors. Ask if the patient has experienced chest pain, labored and painful breathing (dyspnea), or syncope. Occasionally, the enlarged pulmonary artery compresses the left recurrent laryngeal nerve, producing hoarseness. Some patients may describe periods of heart palpitations.
Signs of right ventricular failure are common, such as jugular venous distension, increased central venous pressure, and peripheral edema. Low cardiac output may produce central cyanosis, syncope, or chest pain. Auscultation of the heart may therefore reveal atrial gallop at the lower left sternal border, narrow splitting of S2 or increased S2 intensity, or ejection click at the second intercostal space, left sternal border. When palpating the precordium, you may detect a heave over the right ventricle or an impulse from the pulmonary artery itself. Signs of left ventricular failure, such as systemic hypotension (low blood pressure) and low urinary output, may coexist. Presentation may include hyperventilation, coughing, and eventually rapid breathing (tachypnea) or dyspnea. Initially, breath sounds may be clear or decreased, but you may hear crackles or wheezing.
The patient is experiencing a potentially life-threatening condition that requires the use of complex medical technology. Assess the anxiety level of the patient, and plan interventions to place a minimum demand on the patient’s energy. Support of the patient is essential throughout hospitalization, from routine care such as placement and maintenance of the pulmonary artery catheter to attempts at averting a cardiac arrest.
Nursing care plan primary nursing diagnosis: Impaired gas exchange related to changes in the alveolar membrane structure and increased pulmonary vascular resistance.
Nursing care plan intervention and treatment plan
Primary pulmonary hypertension has limited therapy, and patients tend to have hemodynamic deterioration in spite of therapy. The median survival rate after diagnosis is 2.5 years. Supportive measures include supplemental oxygen for people who are hypoxemic and the use of diuretics in people who are fluid-overloaded. Relief of hypoxemia helps reduce pulmonary vasoconstriction. If the origin of the problem is structural, surgery may be attempted. Heart-lung transplantation is a consideration for severe conditions.
To minimize the risk of infection, use the sterile technique during setup and maintenance of the pulmonary artery catheter. Dressings should be changed according to policy, usually every 72 hours. Ask the patient to evaluate chest pain using a scale from 1 to 10, and provide comfort
measures in addition to any ordered medication. Reduce energy demands by assisting the patient to a position of comfort, such as the semi-Fowler or Fowler position. Document pulmonary artery catheter readings and report significant changes to the medical team. Monitor the patient for the development of cardiac dysrhythmias.
Allow the patient to verbalize fears, and assist in the development of a realistic perception as the patient appears ready. Incorporate family members and other support system members as appropriate. Help the patient adjust to the limitations imposed by this disorder. Advise against overexertion, and suggest frequent rest periods between activities. The patient may need diversional activities during periods of restricted activity. Be sure the patient understands dietary limitations and medication regimens.
Nursing care plan discharge and home health care guidelines
Risk for recurrent pulmonary embolism can be reduced by teaching the patient to minimize hypercoagulability, to reduce venous stasis, and to control risk factors such as obesity. Teach the patient to drink 2000 mL of fluid a day unless restricted, to rest between activities, and to avoid overexertion. Teach the patient about the prescribed dosage, route, action, and follow-up laboratory work needed for all medications. If the patient is discharged on potassium-wasting diuretics, encourage a diet that is rich in high-potassium foods, such as apricots, bananas, oranges, and raw vegetables. The patient may also need instruction on a low-sodium diet. If the patient needs home oxygen, instruct the patient and significant others in oxygen use and oxygen safety. Arrange with social services for the delivery of oxygen equipment. If the patient smokes, teach strategies for smoking cessation or provide a referral for smoking cessation programs.
No comments:
Post a Comment