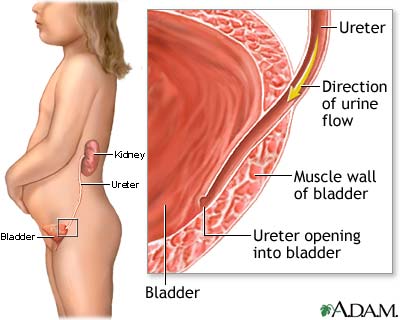
Pyelonephritis is an inflammation of the renal pelvis and of the renal tissue; it is caused by an invasion of microorganisms. More than 200,000 cases are diagnosed each year in the United States. It can be either acute (also known as acute infective tubulointerstitial nephritis) or chronic in nature, as differentiated by the clinical picture and long-term effects. The infection, which primarily affects the renal pelvis, calyces, and medulla, progresses through the urinary tract as organisms ascend the ureters from the bladder because of vesicoureteral reflux (reflux of urine up the ureter during micturition) or contamination.
Acute pyelonephritis occurs 24 to 48 hours after contamination of the urethra or after instrumentation such as a catheterization. Complications include calculus formation, renal abscesses, septic shock, and chronic pyelonephritis. Chronic pyelonephritis is a persistent infection that causes progressive inflammation and scarring. It usually occurs after chronic obstruction or because of vesicoureteral reflux. This destruction of renal cells may alter the urine-concentrating capability of the kidney and can lead to chronic renal failure.
The causative organisms are usually bacteria but can be fungi or viruses. Patients with diabetes, hypertension, chronic renal calculi, chronic cystitis, and congenital or abnormal urinary tract and pregnant women are more likely to acquire pyelonephritis than are other groups. Escherichia coli is responsible for 90% of the episodes in a normal anatomic urinary tract system. Proteus, klebsiella, and occasionally gram-positive cocci account for the rest.
Nursing care plan assessment and physical examination
Question the patient carefully to determine if he or she has experienced dysuria, frequency, and urgency (signs of an irritative urinary tract) before seeking care. Ask if the patient is voiding in small amounts or experiencing nocturia. It is important to determine if these symptoms are a change from the patient’s usual voiding patterns. Ask for a description of the urine, which may be foul-smelling, cloudy, or bloody, and of any pain; discomfort resulting from pyelonephritis usually occurs in the flank, groin, or suprapubic areas. Also question the patient about any flulike symptoms, such as malaise, nausea, vomiting, chills, headache, and fatigue. The pain may radiate down the ureter toward the epigastrium and may be colicky if it is associated with a renal calculus.
If you suspect acute pyelonephritis, determine if the patient is febrile. Inspect the urine for color, cloudiness, blood, or presence of a foul odor. Percussion or deep palpation over the costovertebral angle elicits marked tenderness. Not all of these signs may be present. Lower urinary tract symptoms are absent in approximately 15% of women. Flank pain, tenderness, and fever may also be absent. In chronic pyelonephritis, the early symptoms are minimal. Assess the blood pressure because often these patients present with hypertension. There may be irritating urinary tract symptoms, but they are milder in nature than in acute pyelonephritis.
To prevent permanent kidney damage, acute and chronic pyelonephritis needs to be diagnosed promptly and treated appropriately. Assess the patient’s ability to care for herself or himself, as well as her or his learning capabilities, support systems, financial resources, and access to healthcare. Identify and alleviate barriers to ensure a prompt, efficient plan of care to help the patient regain a sense of wellness.
Nursing care plan primary nursing diagnosis: Infection (urinary tract) related to instrumentation, contamination, or obstruction.
Nursing care plan intervention and treatment plan
The goal of therapy is to rid the urinary tract of the pathogenic organisms and to relieve an obstruction if present. The antibiotics chosen depend on the urine culture and sensitivity. Urinary catheterization is used only when absolutely necessary. Surgery is performed only if an underlying defect is causing obstruction, reflux, or calculi. Hypertension is common in patients with chronic pyelonephritis and needs to be controlled with medication. In addition, supportive care is important. If the cause of pyelonephritis is renal calculi, dietary management, such as limiting calcium, oxalate, or purines, may be necessary.
Provide comfort measures for the patient with flank pain, headache, and irritating urinary tract symptoms. Back rubs may provide some relief of flank pain. Sitz baths may provide some relief if perineal discomfort is present. It is helpful to use a pain management flowsheet and alternative distractions and comfort measures (massage, music, positioning, verbal support, imagery). Because the patient is usually febrile, employ measures that promote heat reduction (cool packs, limited bedding, cool room temperature). To promote nutrition and adequate fluid balance, ask the patient his or her fluid preferences. Encourage the patient to drink at least 2000 mL/day to help empty the bladder and to prevent calculus formation but not more than 4000 mL/day, which would dilute the antibiotic concentration and lessen its effectiveness. Initiate measures to ensure complete emptying of the bladder, such as running water or spraying the perineum with warm water. Ensure the patient’s privacy during voiding.
Teach women in the high-risk groups strategies to limit reinfection. Encourage the woman to clean the perineum by wiping from the front to the back after bowel movements. Stress the need for frequent hand washing. Explain the need for routine checkups if the patient experiences frequent urinary tract infections. Encourage the patient to notify the physician if she notes cloudy urine, burning on urination, and urinary frequency or urgency.
Nursing care plan discharge and home health care guidelines
Instruct the patient on ways to reduce the risk of subsequent infections: increase fluid intake to 2000 to 3000 mL/day to wash the bacteria out of the bladder; avoid caffeine and alcohol; drink juices that acidify the urine (cranberry, plum, and prune); void at the first urge and at least every 2 to 3 hours during the day to prevent bladder distension; void immediately after sexual intercourse and drink two glasses of water as soon as possible; practice good perineal hygiene (wipe labia from front to back). Explain to the patient that the entire prescription of antibiotics should be taken even if the patient feels better. Emphasize the importance of following the special instructions that accompany the antibiotic. Emphasize the importance of follow-up urine cultures and examinations. Note that recurrent infection may require prolonged antibiotic therapy.
No comments:
Post a Comment